11
Jul
Acne Unpacked: The Tells and The Treatments for Acne-prone Skin

I love my skin.
It’s an affirmation and a beautiful sentiment. But for those with acne-prone skin, it is a case of “easier said than done.” Acne affects more than the skin: It can make you feel unattractive. Embarrassed. Self-conscious. Anxious. Along with significant emotional distress which is no less real.
Most people get a pimple now and then, especially in those awkward teen years! But what if you, like 20% of Canadians (that’s five million people!) are struggling with something much more persistent and painful than a passing blemish? There is hope! There are effective medical treatments for acne–prone skin. Let’s explore what it is, why it happens, and how to treat it.
What Is Acne?
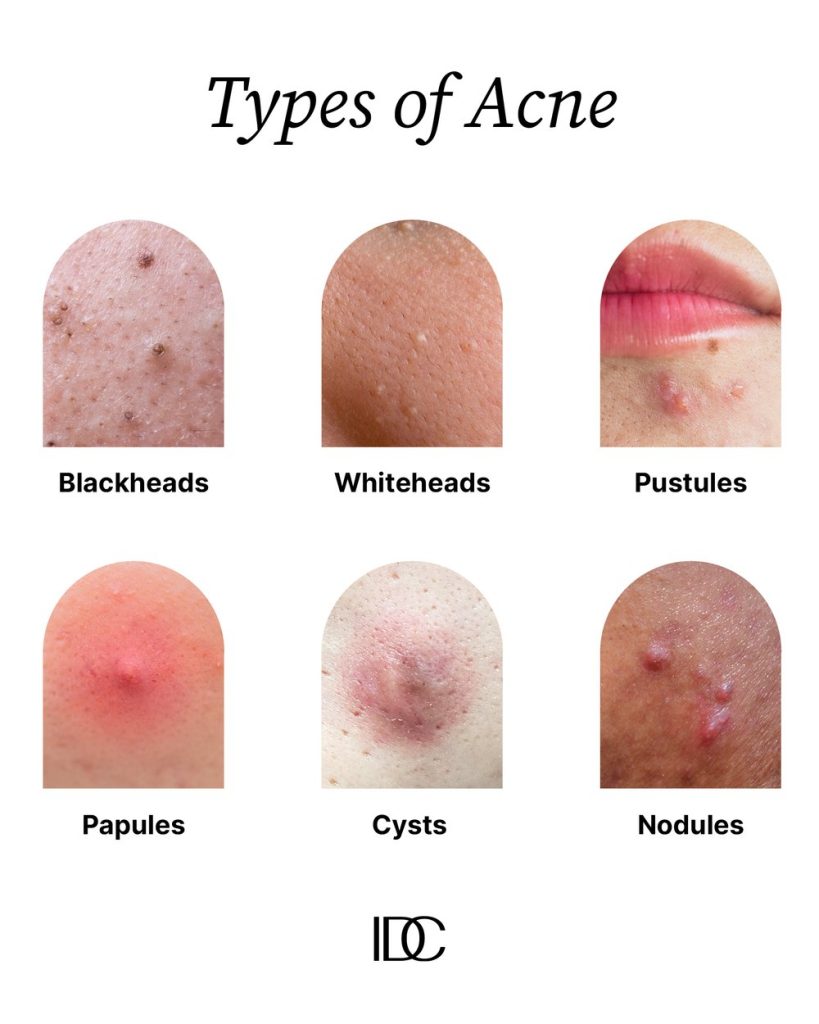
Scientifically speaking, acne is a common condition that occurs when hair follicles get clogged with dead skin cells. This leads to a buildup of sebum: a sticky, oily substance. In “normal” skin, lipid-rich sebum moisturizes and protects. In acne-prone skin, it accumulates. Bacteria in the pores can further block and inflame the pilosebaceous unit (i.e. hair follicle or sebaceous gland) causing unsightly and painful acne, including:
- Blackheads. A.K.A. open comedones. The clogged pore is partially open at the surface, giving that oxidized, “black” look.
- Whiteheads. Unlike the blackhead, these comedones have a layer of skin over their surface. You’ll be able to see the telltale pale white center.
- Pustules. This is a rather unsavory name for a pimple. The clogged pores become swollen, red, and filled with pus.
- Papules. Papules are blocked pores with a small, red appearance. They may feel sore or even rough like sandpaper.
- Cysts. Often large and painful, cysts are akin to boils with pus-filled sacs that extend well below the skin surface.
- Nodules. Like cysts, nodules are often large and painful. The solid, red bumps develop deep in the skin.
The Invisible Symptoms
The invisible symptoms of acne can be just as challenging to cope with; according to a Canadian study published in the British Journal of Dermatology, even mild acne can negatively affect self-esteem and increase feelings of depression. It can also interfere with daily activities and the willingness to (and joy in) socializing and speaking up, among others.
The Three Stages of Acne

Beyond being unpleasant and painful, there are three stages of acne:
- Mild: Here, you may have a few small lesions (which sounds scary but simply refers to an area of affected tissue). These are typically close to the skin surface, and may or may not be inflamed.
- Moderate: People with moderate acne usually see larger and more extensive lesions, in the form of blackheads and whiteheads. These cover more of the face and can be present on the back and chest.
- Severe: Those with severe acne have many more spots, as well as nodules and cysts. They will experience redness and inflammation over much of their face and frequently on the back and chest.
The (Too) Many Types of Acne
Acne isn’t a single condition, there are many different types. These differentiators are critical information because it allows us to treat you effectively.
- Comedonal Acne: This is the “whiteheads” and “blackheads” type of acne that can develop in anyone but is most common in young teens. The comedones (or papules), are either open or closed and typically found on the forehead and chin, making skin appear bumpy and uneven.
- Cystic Acne: This is a severe type of acne that causes pus-filled sacs to form under the skin. In addition to dead skin cells and sebum clogging the pores, bacteria also finds its way in. This causes swelling and inflammation.
- Hormonal Acne: Your hormones can lead to excess sebum production and subsequent clogging of the pores. Biological women are especially vulnerable because of the shifts that occur during pregnancy and menopause. You will usually experience non-inflammatory blackheads and whiteheads.
- Fungal Acne: Instead of a buildup of sebum, people with fungal acne develop excess yeast. Common signs include whiteheads and spots that are red, itchy, irritated, and inflamed.
- Acne-Type Rash: Sometimes, medications or other skin conditions can create an acne-type rash. This is not “true” acne and can be treated quite effectively with over-the-counter products.
It is possible for one person to contend with a combination of different types of acne. Pinpointing the source of the issue leads to the most effective treatment for your unique needs.

Who Gets Acne – and When?
- Teens: Teenagers are most impacted. About 85% of those aged 12 to 24 have acne. This is usually a rough patch of five to ten years, but about a quarter will still have acne at age 25.
- Women: Acne can also begin in adulthood. Again, biological women are disproportionately affected, making up 75% of all cases. This is why many women experience cyclical acne – right in time to signal a menstrual period or during pregnancy and menopause.
- Everyone: The reality is, though, that acne is fairly indiscriminate. It affects women, men, adolescents, and people of all ethnic groups. Five million Canadians (20% of us) cope with acne – and many of us are not getting the targeted treatment we need.
What Causes Acne?
There are several acne-causing factors that we can address, such as:
- Cosmetic Use. Some makeup and hair care products clog pores. Be proactive and look for “oil free,” “non-comedogenic,” or “non-acnegenic.”
- Physical Pressure. Breakouts can concentrate around tight fitting objects, like a bra strap or sports helmet. That pressure can cause acne, so loosen those straps!
- Overwashing. When confronted with acne, a natural urge is to wash more. Cleaning your face more than twice a day is too often. Adding in exfoliating, scrubbing, AND using strong astringent worsens the problem. If you have acne-prone skin, wash twice a day with a mild cleanser.
- Pick and Squeezing. Another natural impulse, but picking at spots both irritates them and sets you up for potential scarring. When you pick or squeeze, it can introduce sebum and bacteria into the tissue, causing more swelling, redness, and even infection.
- Diet. What you eat won’t cure or prevent acne, but it can have an impact. Certain foods, typically dairy and sugars, can aggravate your skin. Consider a low glycemic diet to manage breakouts.
Now, what about the causes and triggers we cannot control?
- Overactive Sebaceous Glands. These oil-producing glands start churning out more sebum, usually during puberty and times associated with hormonal changes like menstrual periods.
- Heredity. If either or both of your parents had/have acne, you are more likely to as well.
- Sweating. Excessive sweating can exacerbate acne in some people. Be sure to change out damp clothing for dry, clean clothes.
- Medications. As mentioned, some medications (e.g. corticosteroids, progestin contraceptive pills, and anticonvulsants) can trigger flare-ups.
Can You Prevent Acne?
Even trying your best, you cannot always, or even usually, prevent acne. Genes and overactive glands can’t be handled with at-home solutions.
Many of those with milder forms of acne find great relief with topical, over-the-counter products. But if you are dealing with a more stubborn, moderate, or severe case, it is time to see your doctor or our board-certified dermatologist for help.
Acne Scarring: More Than Skin Deep
As if acne weren’t troubling enough, the reminders can last a lifetime. Scarring affects one in five people with acne. The risk is highest in those with:
- Severe acne
- Prolonged acne
- A family history of scarring
- A tendency to squeeze or “pop” their spots
Like any scar, this is a result of injury to the skin. With atrophic scars, the loss of tissue creates indents in the skin. These look like little pits. Hypertrophic scars occur when the body is too good at healing itself. Some bodies produce excess collagen to repair the wound creating a raised, thickened knot of skin.
Acne scars are more likely to develop if there is more extensive and longer-lasting inflammation. This is why seeking professional advice as soon as possible is important; it can help you take back your appearance – and confidence
The Impact of Acne
Findings in “Breaking Out: A report on the acne patient experience in Canada,” conducted by the Acne and Rosacea Society of Canada and the Canadian Skin Patient Alliance, revealed that 87% of Canadian acne patients report scarring and 90% say they’ve had changes in pigmentation. CSPA executive director Rachael Manion, says, “Acne is more than skin deep. This is a condition that impacts people’s emotional, social and mental health, going far beyond a cosmetic concern.”
The new study backs up previous research on the emotional impact of acne. Half of respondents said they were “often” or “always” concerned that their skin would never clear up, 44% were “often” or “always” self-conscious about their condition, and 25% avoided social interactions, which is devastating when treatments are available.
When To See a Professional
Should you see a doctor or dermatologist?
- Your acne is getting worse.
- You’ve been using over-the-counter (OTC) products for six to eight weeks and see no change.
- You are having adverse reactions to OTC products.
- You notice scarring and/or dark marks.
- You feel anxious, embarrassed, self-conscious, angry, and/or depressed about your skin.
- You have moderate-severe acne in your family tree.
- There are large, red nodules or cysts under the skin, and they are painful.
- For biological women, you have irregular periods, increased body hair growth, and worsening acne.
- You have extensive acne on your face and, perhaps, also on your chest, back, and shoulders.
If any of these statements are true for you, schedule an appointment.
3 Compelling Reasons Why You’ll Want to See a Dermatologist
Everyone’s acne isn’t the same. Some acne may require medical treatment first. Medical professionals are here to help you figure out the best plan, taking all the options and your unique skin into account.

- They seek out the root cause. Rather than simply treating symptoms (which is undoubtedly important!), a board-certified dermatologist can identify whether there are any underlying health issues that are contributing to or causing the condition. Whether there is or not, they can then recommend the best treatment options for you.
- Your treatment can be medical AND cosmetic. In a world filled with acne treatments, knowing which one is best for you and your skin goals isn’t easy. A board-certified dermatologist can help you wade through the waters of treatment options. You’ll get a plan that works without wasting your hard-earned money.
- You can work on prevention. With our dermatologist’s guidance, you can learn what steps to take to prevent flare-ups, scarring, pigmentation, and how to manage long-term damage.
Treatment Options for Acne-Prone Skin and Acne Scarring
Why see a dermatologist for acne and/or acne scarring? IDC’s own Dr. Dianne Burrows, board-certified dermatologist and fellow of the Royal College of Physicians and Surgeons of Canada, says, “We see a lot [of acne and acne scarring] and understand it from a medical and cosmetic perspective. Some people spend hundreds of dollars on creams and treatments when they really just need to be managed medically (at least at first).”
There are a variety of treatment options for acne-prone skin, but no one-size-fits-all. It’s imperative that you develop a treatment plan in conjunction with medical professionals to ensure accuracy and efficacy. As you build this plan, some cosmetic treatments could include:
- BroadBand Light (BBL). This will sterilize the skin. While not a permanent solution, it can help control acute flare-ups, pimples, and inflammation.
- RF Microneedling. For those with tough cystic acne RF Microneedling is a game-changer. Even better, it can make your skin less acne-prone in the long-term.
- Medical-Grade Skincare. When OTC is not enough, your dermatologist may prescribe medical grade skincare. The concentration of active ingredients is typically higher than their drugstore or department store counterparts.
- Laser Resurfacing. Resurfacing is often used to address scarring; focused laser application can break up scar tissue and stimulate the growth of healthy, new cells.
- Peels. When acne presents with blackheads, whiteheads, and issues with skin texture, a laser or chemical peel can remove dead skin cells and excess oil to reduce clogging and blockages. Advanced peels can address scarring by encouraging help growth beneath the skin’s surface.

Your Skin, But Better
Acne isn’t just one thing and neither are you! Even with acne or scarring, you don’t need to live life weighed down by its emotional and physical presence. There are treatments available. With all this helpful information, you can determine if your doctor or our dermatologist is the right next step. Acne doesn’t present, act, or respond the same way for everyone – you need a solution that works for you.
Here at Interior Dermatology, we’ll help you make that plan and put it into action, so you can have natural beauty and complete confidence. Start your journey to loving your skin today and book an appointment.

Success Stories
Our patients consistently express their heartfelt appreciation for our services and team. We are deeply proud and genuinely delighted to serve such outstanding individuals, whom we cherish and care for as if they were our own family.